Surgery to stop strokes reroutes vessels from torso to brain
(Medical Xpress) -- Five-year-old Ava Menefee was suffering frightening stroke-like episodes: One side of her face would temporarily droop, or she’d lose all sensation in one hand. Although the girl had undergone surgery to fix the faulty blood flow to her brain that caused the episodes, the operation had failed.
Ava’s parents, Scott and Chuan Menefee, knew the problem was dire. The Los Banos, Calif., family had been told another brain surgery was not possible. But Ava’s episodes, called transient ischemic attacks, would likely escalate to full-blown strokes and lasting brain damage unless repaired.
In June, the family’s search for a second opinion led them to Gary Steinberg, MD, PhD, a neurosurgeon at Lucile Packard Children’s Hospital and Stanford Hospital & Clinics, who offered a bold plan to fix Ava’s brain. “When all else fails, you try this,” he said.
Steinberg and his colleague, Sanjeev Dutta, MD, proposed stretching a network of blood vessels in the abdomen up to Ava’s brain. They would leave the vessel network attached to its blood supply in the torso and tunnel the blood vessels under the skin along one side of Ava’s neck to the surface of her brain.
Hearing the plan, Scott and Chuan were relieved — and overwhelmed. The prospect of another brain surgery for Ava “was awful,” Chuan said. And yet the family desperately wanted Ava to be able to return to her favorite activities — from playing softball to riding her horse — unimpeded by transient ischemic attacks or the threat of future strokes. “The only thing worse would have been to hear them say they couldn’t do anything at all,” Chuan said.
Steinberg, professor and chair of neurosurgery at the School of Medicine, is one of the world’s foremost experts in the surgical repair of moyamoya, the name of Ava’s brain vascularization problem. Ava was born without some of the large blood vessels that normally supply the brain. The Japanese word moyamoya translates as “puff of smoke,” a description of the tiny, fragile clusters of blood vessels that the brain grows to try to compensate for the missing vessels.
In her first surgery at another hospital, Ava’s scalp arteries and a scalp muscle called the temporalis had been grafted onto the surface of her brain in the hope that they would take root and replace the missing circulation, a method that works most of the time. But because it failed for Ava, there were no longer any scalp arteries or muscle to use in another attempt at repair.
“I’ve never quite seen this problem before,” Chuan recalled Steinberg telling them at their first visit. “But we can fix it.”
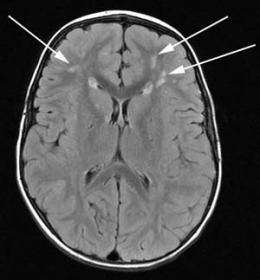
Ava’s transient ischemic attacks had become so frequent that she couldn’t attend school, and an MRI scan showed that she was beginning to experience small strokes as well. Sixty-five percent of symptomatic patients who do not receive surgical repair and have impaired blood flow to the brain suffer major strokes within five years of diagnosis. That high probability of stroke was the reason a second brain surgery was worth the risk.
Steinberg needed blood vessels from Ava’s abdomen, which is why he brought Dutta, a pediatric surgeon, onto the medical team. A specialist in minimally invasive surgery, Dutta could use laparoscopic instruments to dissect Ava’s omentum, a network of abdominal blood vessels found in a large flap of soft tissue near the stomach and liver, away from the organs it normally supplies.
“The approach we planned is very unusual,” said Dutta, who is also an associate professor of surgery and pediatrics at the medical school. The omentum has been used for brain revascularization before, but, to the surgeons’ knowledge, had never been stretched to supply both sides of the brain. In its normal role in the abdomen, the omentum quickly creates new blood vessels at sites of trauma or infection. “That ability is what we’re exploiting in this situation,” he said.
In the operating room, Dutta made four tiny incisions, each less than an inch long, in Ava’s abdomen. With assistance from pediatric surgeon Matias Bruzoni, MD, Dutta separated the omentum from other abdominal organs and then cut its parallel channels in a special pattern to elongate it. He tunneled the vessels up under Ava’s skin, making one more small incision in her neck to help turn a corner in the tunnel. Steinberg performed a bilateral craniotomy and carefully laid the blood vessels on both hemispheres of her brain. The vessels are expected to grow new channels to supply blood into Ava’s brain.
The unconventional approach worked. Now, nearly three months after Ava’s Sept. 15 surgery, her transient ischemic attacks have become much less frequent and severe, a good sign that new blood vessels are beginning to form in her brain.
“Ava’s prognosis is excellent for living a normal life,” Steinberg said.
The uncommon procedure, and the teamwork it required between different surgical specialties, provide “a perfect example of the type of collaboration we can accomplish at Packard Children’s,” Dutta said. “This was a pretty unusual, heroic effort to help this child.”
Ava showed her own heroic side in her recovery, quickly returning to many of her favorite activities. She loves kindergarten, especially reading, and wants to be a teacher when she grows up.
“She’s the toughest, bravest person I know,” Chuan said of her daughter. The 2011 holidays will have extra meaning for the Menefee family, she added. “We’re so thankful because this year, we know how close we came to having a very different life. We’re just fortunate to have a facility like Packard Children’s so close to us, with the kind of people who are here. We know we’re in the very best hands.”

















